BEDSORES – TREATMENT
The best treatment outcomes will result from using a multidisciplinary team of specialists, to ensure all problems are addressed. Units specializing in wound care like Savelegs Diabetic Foot & Wound Care Centre, are able to give better results when compared to other units.
There are six major contributors to healing.
Proper care
The most important care is the relief of pressure. Once a bed sore is found, pressure should immediately be removed from the area and the patient turned at least every two hours to avoid aggravating the wound and preventing the development of newer wounds. Ensuring dry sheets regular changes of linen alongwith the use of catheters or impermeable dressings.
For paralyzed individuals, pressure shifting on a regular basis and use of a pressure relief sheet like a silicone gel sheet,can help prevent pressure wounds.
Pressure-distributive mattresses, water mattresses & Air mattresses are used to reduce high values of pressure on prominent or bony areas of the body.
Debridement
Removal of dead/necrotic tissue is an absolute must in the treatment of pressure ulcers. Dead tissue is an ideal medium for infection and greatly reduces wound healing and the ability of the body to repair itself. Various methods are used to remove such tissue
Autolytic Debridement – the use of moist dressings to promote autolysis with the body’s own enzymes- Though slow it is painless
Maggots – In some countries maggots are used for the purpose but not yet available in India.
Enzymatic Debridement – The use of certain enzymes to promote removal of dead tissue.
Surgical Debridement – The removal of such tissue by surgical means
Mechanical Debridement – The use of mechanical means like pressure water jets to remove the tissue.
Ultrasonic Debridement – The use of ultrasound waves to remove dead tissue.
These modalities may be used individually or in various combinations as the wound progresses.
Infection control
Local as well as systemic infection needs to be controlled. This may involve the use of antibiotics for systemic control and the use of local wound dressings to remove infection locally. The advent of newer dressings like ionic silver has been a breakthrough in this regard.
Once the systemic signs settle, usually the use of oral and parenteral antibiotics is avoided.
Nutritional support
The best diet to support healing is prescribed to such patients, as a malnourished person does not have the ability to synthesize enough protein to repair tissue.Protein levels, leucocyte counts, thyroid profiles and other blood tests may be conducted ,if malnourishment is suspected.
Based on these or clinical exams, the physician may start dietary supplements and various nutrients including parenteral supplements depending upon the condition of the patient.
There is anecdotal evidence that high protein diet helps healing of sores.
Educating the caregiver & Psychological Counselling
If the patient is to be shifted to the house, it is very important to educate the family about how to treat the pressure ulcers. The caregiver should be trained in the proper way to turn the patient, how to properly dress the wound & nourish the patient. If possible a system of online access using technology or domiciliary visits by a trained member of the team should be in place, so that the difficulty experienced by the caregivers in bringing the patient to hospital can be avoided.
Given that these are chronic problems which cause a emotional, financial and mental drain on the family and caregivers, a program of psychological counseling and guidance for them should be adhered to..
Wound intervention
Once the patient has reached the point that intervention is possible, there are many different options.
For Stage I & II sores, usually just removal of pressure and wound care using accepted guidelines in usually enough.
For Stage III & IV ulcers, the use of tissue flaps or other closure methods used to be the treatment of choice. However with the advent of Negative Pressure Wound Therapy, advanced dressing materials and various pressure reducing beds and devices, it may now be possible to close such wounds without major surgical intervention.
These patients need regular evaluation to determine future course of action.
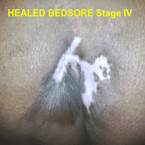
HEALED BEDSORE STAGE IV